The Daily Explains: Interpreting COVID-19 test results at Northwestern
Angeli Mittal/Daily Senior Staffer
A test result is more than what one might see at face value. Northwestern researchers and professors discuss factors to consider and steps to take when taking antigen or RT-PCR.
January 11, 2022
Interpreting COVID-19 tests requires more nuance than reading a red-colored strip on an antigen test. The Daily examined what factors to consider when interpreting results and spoke with Northwestern health experts to understand the nuance behind test results.
Comparing antigen and molecular tests
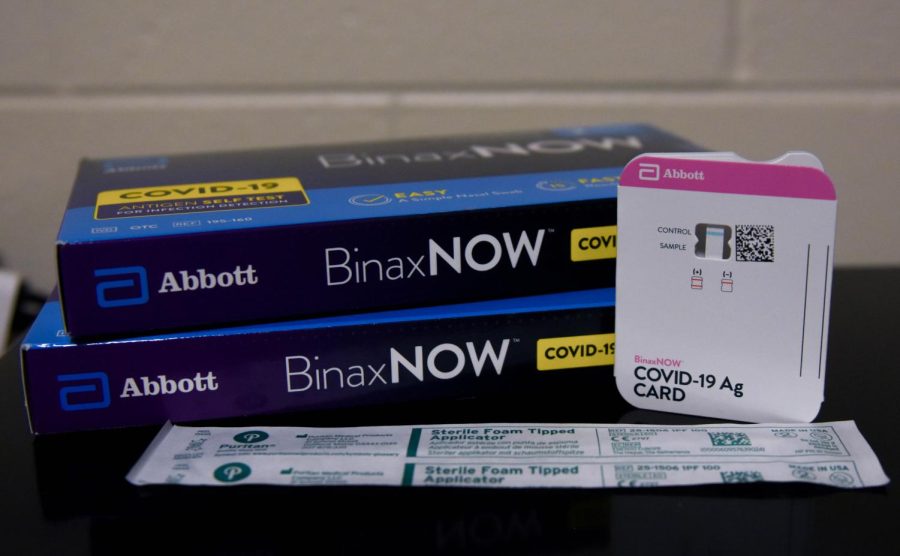
NU administers two types of tests: BinaxNOW COVID-19 rapid antigen tests and RT-PCR molecular tests.
Antigen tests work by identifying the proteins, or antigens, present in viral particles. If antigens are present in the sample, they stick to the antibodies on the strip when the nasal swab sample is mixed with a buffer liquid.
Biological anthropologist and anthropology Prof. Thomas McDade said RT-PCR tests work by identifying the nucleic acids of the SARS-CoV-2 virus — the virus that causes COVID-19 — and converting it to DNA for amplification and detection. Because it doesn’t require a large viral load in the sample, PCR tests can detect the virus more accurately than antigen tests. McDade said antigen tests require a large amount of the virus to be detectable.
“A downside of the PCR test is it’s more expensive … and it can take longer to return the results … that’s a disadvantage if you’re trying to detect someone who might be infectious,” McDade said. “The antigen tests are not as sensitive, so it’s possible to get a false negative result with the antigen test more so than with the PCR test.”
A test’s sensitivity is a measure of its ability to detect the disease. A test’s specificity is its ability to correctly identify those who don’t have the disease.
In the Morbidity and Mortality Weekly Report, BinaxNOW rapid antigen tests reported a sensitivity of about 64% in symptomatic individuals and about 35% in asymptomatic individuals with a 100% specificity in both groups. These percentages are in comparison to RT-PCR testing, which are presumed to be 100% sensitive and specific.
A study published in Annals of Internal Medicine examined the sensitivity of RT-PCR throughout disease progression. The study found the highest sensitivity, 80%, three days after onset of symptoms. However, Feinberg Prof. Richard D’Aquila said it’s unclear how these tests will perform in the context of the omicron variant, especially because most of these tests have been researched with earlier variants and symptomatic individuals.
Factors affecting test interpretation
The proportion of infected people in the population must also be considered. The more infected a population, the more confident someone can be about having COVID-19 if they receive a positive test result.
To mitigate uncertainty that may arise from a test’s low ability to identify infected populations, individuals can consistently test over a time frame. If the tests were performed correctly, then the likelihood of having either a true negative or true positive increases.
Center for Pathogen Genomics and Microbial Evolution Director Egon Ozer said some studies suggest a correlation between high volumes of the virus and infectiousness. However, these studies may be outdated as new variants emerge.
“If only the PCR tests, and not the antigen tests, are positive, (then) in most cases the cells could not be infected in culture,” Ozer said. “The caveat being (these studies examined) older versions of the virus.”
A December study in a preprint server examined the limitations of rapid antigen testing in detecting the omicron variant, especially in asymptomatic individuals. Researchers found rapid antigen tests may produce false negative results in the first two days of being deemed infectious, during which time they would have likely received a positive PCR result.
D’Aquila said while the possible correlation between high viral load and infectivity requires more testing, it may be the correct assumption to make. But he cautions against extrapolating results to asymptomatic individuals.
Negative test results from an antigen test do not rule out the possibility of COVID-19 infection, so symptomatic individuals who receive negative test results should follow up with molecular testing.
If an individual tests positive for COVID-19, the chances of the result being a true positive are high regardless of the type of test. In these cases, NU requires all students, regardless of vaccination status, to self-isolate.
Steps to take after receiving a test result
A study conducted in the U.K. showed about 31% of individuals with COVID-19 remain infectious after five days of a positive test result.
Other researchers found validity in the Centers for Disease Control and Prevention recommendations to shorten isolation for asymptomatic individuals but little benefit in testing five days after a positive test result when the isolation and infectious periods coincide.
Students living on-campus are instructed to isolate in 1835 Hinman for 10 days. If they are asymptomatic five days after initially testing positive, students can end their isolation period pending a negative rapid antigen test result.
D’Aquila said regardless of a negative test result, if someone is symptomatic, they should stay isolated and get another test after at least 36 to 48 hours.
“I tell everyone who has any little symptom — a little scratchy throat, anything — I say you need to keep masked and isolated and use good hand hygiene, because until proven otherwise, it’s probably COVID,” D’Aquila said.
Email: amittal@u.northwestern.edu
Twitter: @amittal27
Related Stories:
— NU clarifies Quarantine & Isolation Housing roommate assignments policy
— NU students in Quarantine and Isolation Housing may be assigned roommates