With no playbook and a finite supply, Evanston health workers must gear up for the long haul
April 25, 2020
In the early weeks of the coronavirus outbreak, emergency medicine physician Michael Slater consulted with the AMITA Health Saint Francis Hospital Evanston ethics team to consider how to ration supplies if the health system reached capacity.
While the hospital has not yet had to use these ethics protocols, Slater said resources are tightening. In efforts to handle the onslaught of patients, St. Francis is constantly reassessing hospital beds, ventilators and personal protective equipment.
“It’s going from adjusting to the chaos of not knowing what’s coming a month ago… now it’s settling for the long haul. From weeks to months of much more difficult work,” Slater said. “That’s a different kind of challenge, of endurance.”
Deep uncertainty around the nature of the outbreak has caused local hospitals to navigate somewhat blindly. When the outbreak first hit the nation, Illinois expected to see the peak number of cases in mid April, according to the University of Washington’s Institute for Health Metrics and Evaluation. Now, new models show Illinois has still not reached ‘peak’ and will not until mid-May, according to Gov. J.B. Pritzker.
As of Friday afternoon, officials reported 39,658 confirmed cases and 1,795 COVID-19 related deaths in the state. The city of Evanston has reported 288 confirmed cases and nine deaths.
Slater and Evanston health care workers have been fighting this pandemic, showing up for shifts every day unsure of when it will end. For as long as the uncertainty remains, so will burdens and stress on regional health care.
Making room for more bodies
In late March, as the virus started to spread like wildfire, Harvard analysis predicted hospitals in Evanston could not handle the projected influx of COVID-19 patients. According to data from the American Hospital Association and the American Hospital Directory, only 670 hospital beds would be available to COVID-19 patients in the Evanston hospital referral region, out of a total 2,030 beds. In order to meet the projected need, hospitals in the region would likely need 2,010 beds for COVID-19 care over 12 months, three times the available beds.
In fighting COVID-19, hospitals provide care for the area far beyond the zip code of the facility. The Evanston hospital referral region is defined as the regional health care market for third-party medical care, which stretches from the Chicago border to North Chicago and as far west as Palatine. Both Evanston hospitals — St. Francis and NorthShore Evanston Hospital — take in many COVID-19 patients that are not Evanston residents.
Researchers estimated over 60,300 coronavirus patients would seek hospital care in the Evanston area. The statistics assume 40 percent of adults will become infected over 12 months, based on infection rates of past pandemics, and that 20 percent of the infected will need hospital care, as was seen in Wuhan earlier this year.
In a lot of ways, the March predictions were the worst-case scenario. The model did not factor in the ability to minimize the number of non-COVID-19 patients nor the ability to expand capacity.
The takeaway was clear: If hospitals did not make changes and the virus followed global patterns, the city of Evanston, and the rest of the country, would run out of beds. In response to capacity predictions, hospitals in Chicago and Evanston began canceling non-emergency surgeries and procedures, which freed up hospital space and increased capacity for care.
Evanston’s local hospitals each belong to their own health system across the city hospital referral area. In developing a COVID-19 preparedness plan, the hospitals in a particular health system function as one team. A pool of medical resources extends to each hospital in the network, which naturally allows for more flexibility.
On April 1, NorthShore converted Glenbrook Hospital, located in Glenview, into its designated COVID-19 site because of the facility’s physical configuration and capacity benefits, said spokesman Carolyn Starks. Intensive care units, the emergency department and inpatient units at Glenbrook have all been converted into “negative pressure environments,” or isolatory measures taken to contain the disease on a room-to-room basis.
NorthShore is admitting COVID-19 patients to Evanston Hospital as needed, depending on the volume and capacity at Glenbrook.
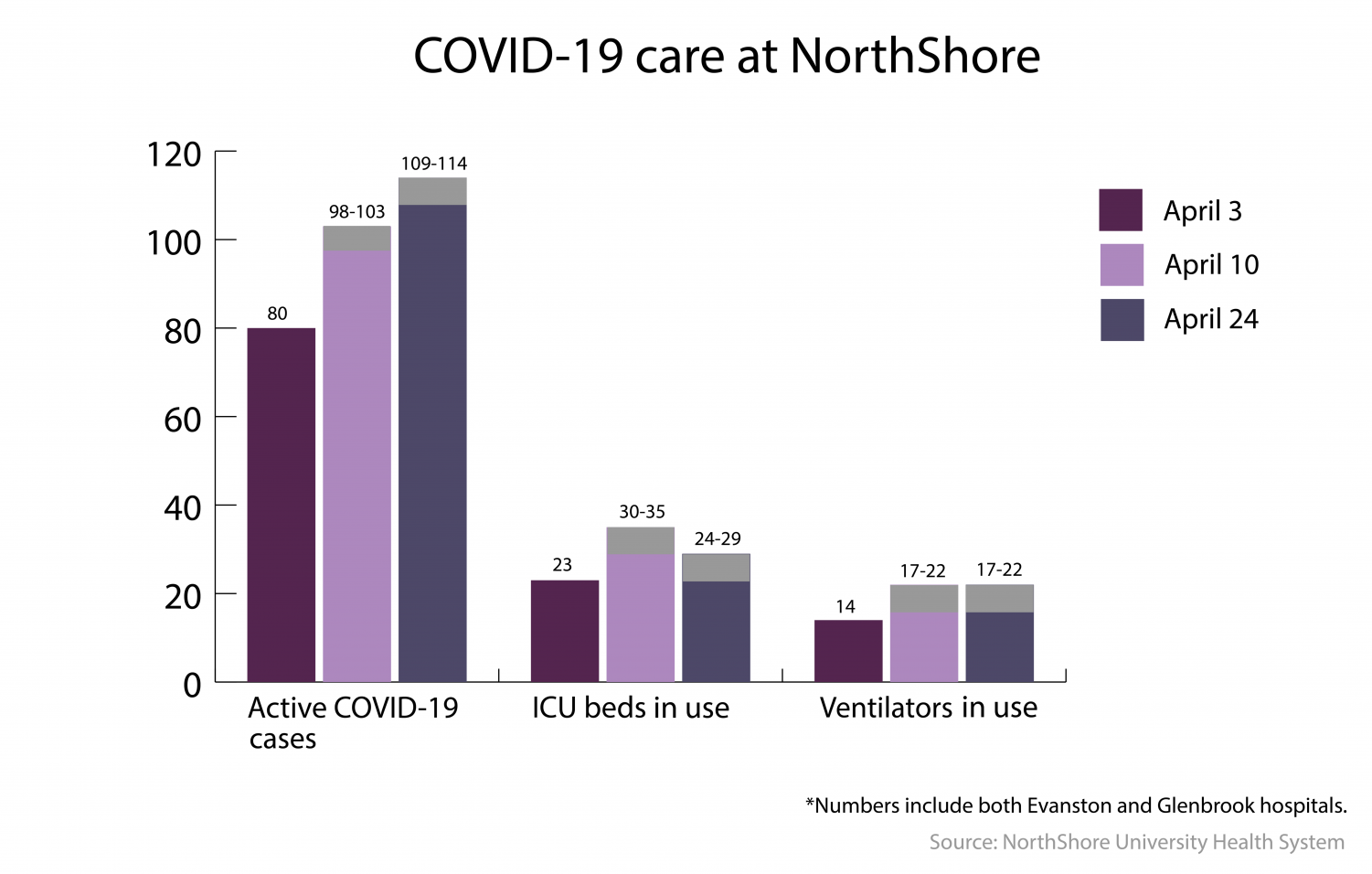
On Friday, Evanston Hospital president Doug Silverstein told the Daily that 109 to 114 patients were receiving COVID-19 care. About 24 to 29 of those patients were in intensive care, well under the capacity of 96 ICU beds.
The NorthShore health system has a total of 527 staffed beds at both sites — 173 staffed beds at Glenbrook and 354 staffed beds at Evanston. Evanston Hospital has the maximum number of beds licensed to operate. There is no potential increase in bed capacity at the site, according to data from Definitive Healthcare. Information was unavailable about the Glenbrook location.
Currently, NorthShore also has an adequate supply of ventilators. As of Friday, only about 17 to 22 patients were on ventilators under a capacity of 150 ventilators, according to Silverstein.
At St. Francis, Slater said he is seeing more and more patients come into the emergency room with COVID-19. As of Thursday, the hospital had cared for a total 353 COVID-19 patients, the second highest within the AMITA Health system.
The hospital has enough beds, but Slater said health care workers are getting sick and cannot come into work. This past week, the hospital has had to transfer some patients to one of the other 13 Chicagoland hospitals within the health system.
“It has been tighter in the last week…It’s kind of up and down day by day, but we’re managing,” Slater said. “There are other places that can offload. That’s been hard but also we’ve had good solutions.”
In preparing for the virus, the hospital overhauled their facilities. St. Francis went from two to 21 ICU isolation beds in the span of one week, which included reopening a closed 9-bed intensive care unit. In an effort to contain the virus, the hospital has also dedicated one floor to COVID-19 ICU care and another floor to non-COVID-19 related care.
The hospital is currently using 14 of the 19 available ventilators, Slater reported. If the need for ventilators grows, the hospital could rely on the 89 ventilators available within the health system.
The need for alternative care facilities is determined at a state level by the Illinois Emergency Management Agency, Illinois Department of Health and the governor’s office, who all receive updates from every health care system in the Evanston hospital referral area. Mayor Steve Hagerty said currently, the state has not yet identified the North Shore area as in need of an alternative care facility.
Nonetheless, the city of Evanston has already identified sites that could serve as alternative care facilities if Evanston’s local hospitals reach capacity. Hagerty said the city has cots set up in a gymnasium in the Chandler-Newberger Community Center, near Evanston Hospital.
Currently, the state has selected four sites in the Chicagoland area to function as temporary alternative care facilities, the closest being McCormick Place, which is about 16 miles from Evanston.
The scramble for PPE
For health care workers on the frontlines, personal protective equipment (PPE) is a barebones safeguard from the invisible disease. When doctors went without gear in Italy, dozens sickened and died.
Like most challenges amid the pandemic, maintaining a PPE supply is an effort health care workers are facing around the country. 20 miles away in downtown Chicago, Terry Strzelczyk, a nurse practitioner at Northwestern Memorial Hospital, said she and health care workers in the COVID-19 intensive care units will reuse their masks until they tear.
N95 masks are effective for up to 8 hours, according to the Centers for Disease Control and Prevention. But health care workers across the country have been reusing masks beyond the recommended time frame to conserve them due to finite supply.
NorthShore is already struggling with maintaining sufficient PPE supply. At the city’s coronavirus task force meeting on Tuesday, Silverstein reported N95 masks would run out in just five days and isolation gowns would run out in one week.
Just days before, on April 21, Silverstein told the city the hospital PPE supply was “adequate.” NorthShore has declined to comment on efforts at restocking.
At St. Francis, use of surgical masks and N95 masks has doubled in recent weeks. To date, the PPE supply is stable at the hospital and health care workers are able to use one mask per shift. Gown supply is “getting tight,” but Slater said the hospital is working on new sources and solutions.
When it comes to personal protective equipment, government on every level in Illinois is scrambling to find PPE. Pritzker has partnered with in-state manufacturers and biotech companies, purchased any supplies available on the market and publicly called on White House to send additional equipment.
“The governor and the Illinois Department of Public Health… are literally scouring the planet for supplies,” Danny Chun of the Illinois Health Hospital Association told the Daily. “The state has been working on procurement contracts from all over the world to secure millions of masks, gowns and gloves.”
Here in Evanston, public health manager Greg Olsen said the city is tasked with maintaining adequate PPE supply in multiple local sectors — at local hospitals, but also at congregate living facilities and at the police and fire departments and other emergency responders. The city regularly decides to whom its limited PPE supply should be distributed and by how much.
Olsen said when local hospitals are low on personal protective equipment, their health systems have their own channels to refill supply. Hospitals, Olsen explained, get personal protective equipment directly from the state.
Right now, Olsen said the city is focused on providing personal protective equipment to congregate living facilities like nursing homes, an effort to prevent a cluster outbreak of COVID-19 cases. The city has already provided PPE to the retirement community Three Crowns Park, which has seen nearly fifty percent of the entire city’s COVID-19 related deaths.
“It’s just a constant battle to make sure that we have enough and, and also, it’s dividing up how much we give to each one based on their specific needs,” Olsen explained.
Email: [email protected]
Twitter: @snehadey_

